|
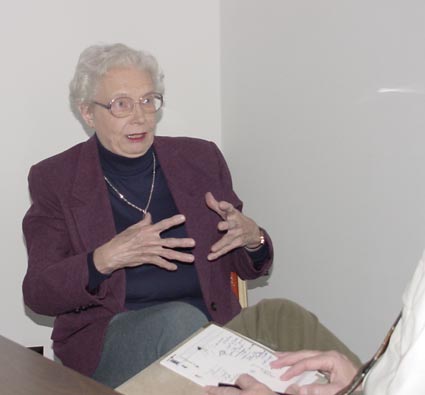
I have attended several seminars on substance abuse and treatment for those
addicted or who are also suffering psychological disorders. Dr. King served as
the medical authority for these workshops. She impressed me with her depth of
knowledge, sensitivity to those in treatment, and her commitment to provide for
the best care and treatment of those in need. You will enjoy getting to know
Dr. Lucy King.
 Al: Lucy, I would like to know something about you personally, where did you go to
school, what did do for a living, and how you are spending your retirement.
Al: Lucy, I would like to know something about you personally, where did you go to
school, what did do for a living, and how you are spending your retirement.
Lucy: I did my training at Washington University in St. Louis: undergraduate,
medical school, and psychiatry residency. Then I stayed on as a faculty member
of the Department of Psychiatry in the medical school. Then went to the faculty
Medical College of Virginia; then worked for the Food and Drug Administration.
Later, I was in private practice of psychiatry and addictions psychiatry in
Manassas, Virginia. For the past ten years, I have been in Indianapolis.
Al:
Why did I think you were in Bloomington at one time?
Lucy: Well, people think that Indiana University is there, but the medical
school is in Indianapolis.
Al:
Why did you choose psychiatry?
Lucy: Washington University at that time was somewhat ahead of its time in
psychiatry in the United States. It was already interested in neurochemistry
and genetics. So, it was an opportunity to be involved with patients and to be
involved with science.
Al:
Were you one of the first women psychiatry?
Lucy: No. Women psychiatrists go back to the 19th century.
Nevertheless, there were not many women in medical school when I was. There
were only three women in my class of about ninety in the 1950s. However,
psychiatry has always had a fair number of women. Most women went into
psychiatry, pediatrics, and obstetrics. At least half the medical students in
the 21st century are women, and they enter all the specialties of
medicine.
 Al: You told me the other day that you recently retired that you went back to work
writing a book. Can you give my readers some information about it?
Al: You told me the other day that you recently retired that you went back to work
writing a book. Can you give my readers some information about it?
Lucy: The title of the book is From Under the Cloud at Seven Steeples.
It is based on a book that was written by a patient at Indiana Hospital for the
Insane in Indianapolis in 1880s. I took her book, which is a very interesting
story of her seven years there, added some comments about psychiatry in the 19th
century, and brought it up-to-date through 20th century. I also talk
a little about psychiatry today, the problems of healthcare delivery, and
getting adequate treatment for people. It's being published by Guild Press and
is coming out in April 2002.
Al:
How is it going to be marketed, and will it be for professionals or for lay
people?
Lucy: Both. It's written so that a layperson could understand it, but I think
it would be of interest to all professionals in the mental health fields. It is
a history, and many of us don't know a great deal about the history of
psychiatry. We know there were asylums, but there were a lot of misconceptions
about treatment back then. I think that my book is really a fun read for
professionals and an interesting read, I hope, for the lay public and people
interested in history.
Al:
Are you working on any other books?
Lucy: No. However, I'm interested in the field of healthcare delivery,
particularly in mental health and addictions. We just don't provide good
healthcare for everybody. So, I'm thinking of doing some writing along that
line. There's an enormous amount written in this area already.
Al:
Would you like to speak a little about the relationship between Anna Agnew's
illness and her creativity?
Lucy: There was an interesting study done at the University of Iowa by Dr.
Nancy Andreasen, and of course, the connection between creativity and bipolar
disorder has been made well known by Dr. Kay Jameson who has written not only a
scientific work on research, but also some very interesting books about bipolar
disorder and creativity.
When I retired in 1999, I started as a volunteer at
the History of Medicine collection at Indiana University Medical School Library
and the librarian there, then, Nancy Ackerman, called my attention to this
book. I read it and got interested in 19th century asylum reform
literature. There is a lot of it out there: pamphlets, books, newspapers. Mrs.
Eckerman sent around to every library we could find that would send us a 19th
century book written about a mental asylum patient who was not famous but just
an ordinary citizen. We got seven books written by eight authors. Part of what
I was interested in was what their diagnosis was. I really didn't know at the
time.
 It turns out that six very clearly had bipolar
disorder and the other two might have. I was somewhat surprised by that, and
then went back and looked at other literature. There does seem to be an
association between bipolar disorder and creativity. A lot of well-known
musicians, writers, poets, and artists suffer from bipolar disorder. However,
the books we looked at were by ordinary people. I think one reason is because
their illness remits, so they write when they are well. The thing that I
enjoyed about the book that was written by the patient that write about was that
it wasn't just a polemic. Usually, people are complaining about abuses-with
excellent reason. She tells the awful stuff and the good stuff. She gives us
an insight into the everyday life in the asylum, and she was not only there when
there were some very abusive practices but also when there was reform. There
was a physician named Dr. William Fletcher, and like all of the doctors she
mentions, this doctor had been in the Civil War. He was a great reformer. He
took all the restraints in the hospital and burned them in a giant bonfire on
Christmas Day of 1883. It made all the newspapers around the Midwest. She
described this. Dr. Fletcher brought in many reforms. He hired the first woman
doctor at the hospital. There were only twenty-two women doctors in state
mental hospitals around the country in the 1880s.
It turns out that six very clearly had bipolar
disorder and the other two might have. I was somewhat surprised by that, and
then went back and looked at other literature. There does seem to be an
association between bipolar disorder and creativity. A lot of well-known
musicians, writers, poets, and artists suffer from bipolar disorder. However,
the books we looked at were by ordinary people. I think one reason is because
their illness remits, so they write when they are well. The thing that I
enjoyed about the book that was written by the patient that write about was that
it wasn't just a polemic. Usually, people are complaining about abuses-with
excellent reason. She tells the awful stuff and the good stuff. She gives us
an insight into the everyday life in the asylum, and she was not only there when
there were some very abusive practices but also when there was reform. There
was a physician named Dr. William Fletcher, and like all of the doctors she
mentions, this doctor had been in the Civil War. He was a great reformer. He
took all the restraints in the hospital and burned them in a giant bonfire on
Christmas Day of 1883. It made all the newspapers around the Midwest. She
described this. Dr. Fletcher brought in many reforms. He hired the first woman
doctor at the hospital. There were only twenty-two women doctors in state
mental hospitals around the country in the 1880s.
The patient Anna Agnew told us the name of her
hometown, Moscow, Ohio, and the first names of a few of her relatives.
Lynn Orvis, who is a genealogy researcher working with
the history of medicine collection, helped me to go around to libraries and
archives to find out about this woman's family. It's been an interesting
quest. She and Nancy Eckerman, the librarian, have compiled biographical
material on 19th century Indiana physicians. When this patient
mentioned her doctors, and we were able to know who they were.
 Al: What do you think the patient/author's motivation to write her detailed journal
of her life at the time in the asylum?
Al: What do you think the patient/author's motivation to write her detailed journal
of her life at the time in the asylum?
Lucy: I think the motivation for all of these people was for reform.
Originally, the asylum was a place of safety and peace away from the cares of
the world. They had lovely gardens and might have a farm where people could
work. They had all kinds of things to do-what we call recreation therapy
today. That was fine as long as there were just a few hundred patients, but
with immigration, urbanization, and an increasing population, these institutions
held thousands of patients and might only have half a dozen doctors and a few
registered nurses. Like all state facilities, they had to depend on tax money.
If there was enough money, they hired staff who were well trained. If there was
not enough money, the staff were untrained and underpaid. People without any
training would sometimes just not know how to handle sick patients and might be
very abusive. There was no medication and little effective treatment at the
time.
Her plea was to the state legislature that they would
make reforms and require that all people who worked with mental health patients
would be trained nurses. We still have that problem today. It's much improved,
but there are still abuses; there is still low pay and lack of training in some
instances.
Al:
I know there had been some treatments, like electroshock. Were there other
treatments that were prevalent in that institution other than just the
warehousing of patients?
Lucy: Electroshock was not introduced until the late 1930s. Warehousing was
never considered a treatment. It was a result of overpopulation, and the
treatment they had went back to the middle 1700's. Philippe Pinal in France
freed mental patients who were chained to the walls and living in terrible
conditions. He invented something that he called "treatment morale," which is
translated into English as "Moral Treatment," but it doesn't mean "moral" as
much as "morale." The theory was that we should treat people kindly, provide
them activities, and respect them. It is really the beginning of
psychotherapy. It is a little bit of a forerunner to cognitive-behavioral
therapy, and that worked fine as long as you didn't have a whole lot of
patients. But with the increases in population and urbanization, you had
2,000-3,000 patients in these institutions. The superintendent just could not
keep up with what was going on. Although they were dedicated, kind attendants
in spite of their difficult jobs, abuse appeared at all levels of staffing.
Anna Agnew described one physician who was horrible and of course, the doctor
hid this from the superintendent. But, the goal was moral treatment. The goal
was never warehousing. This was an unfortunate consequence of too many people.
As in the care today, we don't want to pay more taxes; therefore, state
institutions are often left with very meager budgets.
 Al: Give me an idea without giving me the end of the story what her day would be
like?
Al: Give me an idea without giving me the end of the story what her day would be
like?
Lucy: Okay. The phone would ring on the ward. They would get up. She
describes this kind of thing, and it is what makes the book so interesting. I
include most of her descriptions. They would get up around 5:30am. They would
all get cleaned up. They had plenty of hot water and soap, they would all get
ready, get prepared, and of course, in the 1880s women had a lot of clothing to
deal with. There would sometimes be arguments among the sicker patients as to
whose dress was whose and that kind of thing. Then they would fall to and clean
up the ward. Then they would have breakfast in the dining room. Those, who
were feeling better, if they so desired, could go to the sewing room. All of the
linens, all of the clothing from the hospital were made in the sewing room.
There people whom they hired, but the patients could also participate in this.
This patient was a skilled seamstress, and so she enjoyed that when she was
feeling better. There is a record of all the patients' clothing in the annual
reports of the hospital. If the patient was indigent, their county would pay
for it. If patients could afford it, their families could send in clothing or
send in yard goods for clothing to be made in the sewing room.
Now, Fletcher in particular, but also some of the
other superintendents, had a drama club and similar activities. Patients had a
piano, and they would play and sing. They had beautiful grounds. That was part
of the moral treatment. They had a farm that not only provided food, but
patients could work there as their recreational activity. They made some sewing
and crafts which were sold and brought in a little bit of money, and some of the
doctors in the better days, would actually spend time talking with them. It was
both a follow-up on moral treatment and a predecessor of what would happen in
the 20th century. However, overcrowding increased, and things got
out of hand.
 Al: Is the building or institution still in existence?
Al: Is the building or institution still in existence?
Lucy: That hospital was closed in 1994 because of allegations of abuse of
patients by staff. There is one of the old buildings left-the pathology
building-which was built in the 1890s and was the state of the art at the time.
It was only the second one in the U.S. to study the brain in psychiatry. For
fifty years, it was the teaching and research location for the Department of
Psychiatry of Indiana University. It is now the Indiana Medical History
Museum. It is a beautiful 19th century building with a lot of
fascinating exhibits. They have a classroom with woven cane-bottom chairs.
They did some research there, which is now antiquated, but it was
state-of-the-art for its time. If you are ever in Indianapolis, go and see it.
Al: Where is it actually located?
Lucy: It's at 3045 West Vermont, west of the Indianapolis Zoo on Washington
Street.
Al:
Regarding our time, I would like your opinion about mainstreaming. What is your
feeling about putting people out of the old state hospitals back into the
community?
Lucy: It depends entirely on the individual patient. It depends on what
illness they have. Is it severe, a chronic mental illness? Do they have a
family support system and does the community provide support? This
mainstreaming started in the 1950s when we first had antipsychotics drugs.
There was effective treatment for the first time. There is an interesting
article in the 1996 "Psychiatric News" by a sociologist named Leona Bachrach who
has studied this issue. For some people, outpatient treatment in the community
has worked. If you have a really good support system, a mental health clinic
that follows these people, case management, help with getting a job, all the
things they need in a community, it can work very well and for some people it
has. In other situations, because our health system is so fragmented, it
doesn't. There are still a few people for whom you can't do a great deal,
although we can do more now than they did then. I think what we have gotten
into is either "everybody goes in the hospital for a long time" or "everybody
comes out of the hospital," and that just doesn't work. I think we still need
long-term supervised care for lots of people, but it depends on the individual.
There are all kinds of options like intensive outpatient programs, daycare,
residential care, etc.
 Al:
What is the societal responsibility for people who do not want to be
institutionalized. We refer to them as street people who are at risk but are
reluctant to accept treatment or assistance. Al:
What is the societal responsibility for people who do not want to be
institutionalized. We refer to them as street people who are at risk but are
reluctant to accept treatment or assistance.
Lucy: There are many programs addressed to these people. Treatment teams
actually go out into the community where people are. The problem is that there
are just not enough of them, and they are not coordinated. This is part of a
much bigger problem; it's the whole healthcare system in America. It is so
fragmented. We have patients with different insurance companies, Medicare,
Medicaid, and indigent people working hard but not having benefits.
There was a very interesting review of this by the
Institute of Medicine, which is part of the National Academy of Sciences, a
quasi-governmental organization that provides scientific medical data to
Congress and the Executive. They published a book which is on the Internet at
http://www.aami.org/subject/safety/ and you can also purchase it.
It's called Crossing the Quality Chasm: American Healthcare in the 21st
Century. It addresses all the problems of all healthcare and makes some
suggestions. There are many groups working on this issue--very recently, both
the AFL-CIO and the Chamber of Commerce have come together about this issue.
The Robert Wood Johnson Foundation has given a lot of money to exploring these
healthcare issues. Lots of people are thinking of healthcare reform. In the
long run, from a purely selfish standpoint, it would cost us much less to have
this coordinated and to provide care to everybody that needs it. Each political
party is in debt to a particular special interest groups, and we saw the whole
uproar about the healthcare reform about ten years ago. Nobody wants to pay
more taxes, etc, but the thing is getting it all coordinated so that good care
is provided at the lowest possible cost. What is the bottom line? There is the
cost to society, the cost to the criminal justice system, the cost to everybody,
etc. Any citizen who is interested should get involved. In the mental health
field, it's the National Alliance of the Mentally Ill, the National Mental
Health Association. Both have local chapters. With bipolar disorder there is
the National Depressive and Manic Depressive Association which has headquarters
in Chicago.
 Al: Is there a specific country that would be a typical model for America?
Al: Is there a specific country that would be a typical model for America?
Lucy: It's very interesting and again, I have some biases. I am in favor of a
national health service; I'm a member of Physicians for National Health Program.
The Canadian system is pretty good, and I think that is probably the closest.
If you have a national health system, and you really cut costs, you limit
access. If you have access, it costs more. Switzerland has a program similar
to ours but reaches people a little bit more and cost less. Germany and France
have programs where there is government-supervised insurance. The insurance
companies aren't making large profits and are somewhat government controlled.
However, they are not charging high fees, physicians are paid much less, and
patients have an access to care and a quality of care in Germany and France that
is unheard of in this country except for the well-to-do.
 I had the experience last fall of falling and breaking
my kneecap. I had to be in the hospital four days and have surgery. Now, as a
physician, I am very accustomed to hospitals and know how to deal with the
system. I was at a university hospital, had excellent care; a coordinator came
into set-up outpatient stuff, but she didn't get there the last day. The
physical therapist came, but not until the last day. So, when I got home, I
started calling around over a few days and finally found out that I was in their
computer; the people at the hospital got in touch with somebody else, who got me
in touch with somebody else. I finally got a nurse to come in and check the
dressing, got a physical therapist, but they didn't do basic home healthcare. I
have steps in my home, and the orthopedic surgeon was upset about my using them
with a leg immobilizer and crutches. I just wanted someone to come in to help
me with that, and we got another group to get a home health aide who came in and
helped me with chores. How many sixty-nine-year old women in this country have
this kind of care? I had "Cadillac" care, but the majority of people in this
country do not. Even with the best possible care, it is fragmented. It was
only because I'm a fussy old maid and got in there and screamed and yelled that
I got it organized for myself. However, this is not available to people who may
be working very hard, but have terrible health care benefits. I know the
system; I've worked it for forty years. I thought, my gosh, this is wonderful
for me, but what about all the others?
I had the experience last fall of falling and breaking
my kneecap. I had to be in the hospital four days and have surgery. Now, as a
physician, I am very accustomed to hospitals and know how to deal with the
system. I was at a university hospital, had excellent care; a coordinator came
into set-up outpatient stuff, but she didn't get there the last day. The
physical therapist came, but not until the last day. So, when I got home, I
started calling around over a few days and finally found out that I was in their
computer; the people at the hospital got in touch with somebody else, who got me
in touch with somebody else. I finally got a nurse to come in and check the
dressing, got a physical therapist, but they didn't do basic home healthcare. I
have steps in my home, and the orthopedic surgeon was upset about my using them
with a leg immobilizer and crutches. I just wanted someone to come in to help
me with that, and we got another group to get a home health aide who came in and
helped me with chores. How many sixty-nine-year old women in this country have
this kind of care? I had "Cadillac" care, but the majority of people in this
country do not. Even with the best possible care, it is fragmented. It was
only because I'm a fussy old maid and got in there and screamed and yelled that
I got it organized for myself. However, this is not available to people who may
be working very hard, but have terrible health care benefits. I know the
system; I've worked it for forty years. I thought, my gosh, this is wonderful
for me, but what about all the others?
I think both healthcare professionals and patients are
angry. The problem is how you get this complicated system together, and there a
lot of people with different interests all lobbying about this. Nevertheless,
America can do a lot of things; I'm always hopeful. In this country, if you
have the money and if you know how to work the system, you get the best
healthcare in the world. However, that's only for a small percentage, and a lot
of people just aren't getting it. People without the money go into emergency
rooms because they can't afford everyday care. That's the most expensive
possible way of providing healthcare. It's costing everybody, and it's not
helping patients as much as if they had regular follow-up, regular physicians,
etc.
 Al: And the thing is that we will see that healthcare cost in our insurance premiums to us directly.
Al: And the thing is that we will see that healthcare cost in our insurance premiums to us directly.
Lucy: Yes. and now that budgets are a little bit tight and states are cutting
back, I really fear for these people.
Al:
Gene Siskel used to ask his interviewees to name their favorite movie. He
thought that would reveal something about them that he couldn't have gotten with
regular interview questions. I have developed my own question: when you croak,
and somebody is in charge of putting your epitaph on your tombstone, how would
you want to be remembered.
Lucy: I prefer not to have an epitaph.
Al: Okay. Well, just suppose...
Lucy: You want my two favorite movies? One is an old one that came out in the
60's or 70's with George C. Scott called Hospital. It's incredibly
funny, but it's a very dark humor picture. He is a hospital administrator. The
other is a recent one, Traffic. I am interested in addictions, but it is
NOT a nice movie. It's harsh, but I think it is very true.
Al:
What is it that you would want people to learn, that you have learned, but that
you could pass on to them so they don't have to reinvent the wheel.
Lucy: Psychiatric disorders and substance dependence are diseases like any
other disease, and these patients as well as all patients, should be treated
with compassion. We fluctuate in our treatment. We lock people up and beat
them, and then we let them all out and treat them nice. We have done this for
thousands of years.
 Al:
It was interesting, the group got into a little bit of a heated discussion about
whether or not alcoholism was a choice.
Al:
It was interesting, the group got into a little bit of a heated discussion about
whether or not alcoholism was a choice.
Lucy: After the first drink, it is not a choice. It depends on inherited
abnormalities in brain chemistry as well as some environmental factors-a
predisposition to substance dependence. However, that choice for the first
drink is made when people are ten, twelve, or sixteen. You know, when I was a
teenager, it was real "sophisticated" to smoke. It still is. Smoking and
drinking are a passage into adulthood. Back when I was young, Bette Davis was a
movie star. I loved to see Bette Davis, and she smoked! I thought,
everybody in the world is really sophisticated if they smoke, and I tried
smoking. But, I made the mistake of looking in the mirror, and I looked
stupid. I thought, well everyone else looks sophisticated, but I look stupid.
Looking into the mirror may have prolonged my life by many years. I was
seventeen, I didn't go to the library and research it, and at that time, we
didn't have all the data about lung cancer. My decision was not thoughtful, it
was not an intellectual, careful, left-brain decision. It was a teenage
decision. That's when people make those choices, and if they have the
predisposition to substance abuse, they are hooked.
The following is the publisher's news release for Dr.
King's new book.
FROM UNDER THE CLOUD
AT SEVEN STEEPLES
The Peculiarly Saddened Life of Anna Agnew at Indiana
Hospital for the Insane, 1878 - 1885.
By Lucy Jane King, M.D.
As Anna Agnew's carriage drew near to the hospital she hoped
would cure her mental illness, she noticed seven steeples (really
eight but the final one could not be seen from the road) pointing
towards the sky. The steeples were a landmark which, seen from the
road approaching the state capital, would locate the place of
refuge or "asylum" for the mentally disturbed committed by law to
the hospital. Anna's experience over the next seven years in Seven
Steeples (Indiana Hospital for the Insane, later Central State
Hospital) under a variety of superintendents and a variety of
treatments is really a chronicle of the history of Frank Zwara,
artist the "insane" in America. In Indianapolis as Collection of
the Indiana Medical History Museum elsewhere, poorly paid young
working class women served as attendants, and some of them beat
and restrained Anna. Cruel treatment was just as common for her in
her years at Seven Steeples as efforts to understand her problem.
Anna suffered from severe mood swings, now called bipolar
disorder. When Anna emerged from Seven Steeples, she wrote a book
which gained a national readership and made her an advocate for
mental health reform. Dr. King, herself a psychiatrist, has
interpreted Anna's story for the modem reader in this fascinating
book, which documents a history from Anna's time to the present of
people and problems too often misunderstood.
ISBN 1-57860-106-1 Hardcover, 185 pp. Retail $24.95
Guild Press Emmis Publishing
Zionsville, IN
APRIL 2002
|
|







 Al: Lucy, I would like to know something about you personally, where did you go to
school, what did do for a living, and how you are spending your retirement.
Al: Lucy, I would like to know something about you personally, where did you go to
school, what did do for a living, and how you are spending your retirement. Al: You told me the other day that you recently retired that you went back to work
writing a book. Can you give my readers some information about it?
Al: You told me the other day that you recently retired that you went back to work
writing a book. Can you give my readers some information about it? It turns out that six very clearly had bipolar
disorder and the other two might have. I was somewhat surprised by that, and
then went back and looked at other literature. There does seem to be an
association between bipolar disorder and creativity. A lot of well-known
musicians, writers, poets, and artists suffer from bipolar disorder. However,
the books we looked at were by ordinary people. I think one reason is because
their illness remits, so they write when they are well. The thing that I
enjoyed about the book that was written by the patient that write about was that
it wasn't just a polemic. Usually, people are complaining about abuses-with
excellent reason. She tells the awful stuff and the good stuff. She gives us
an insight into the everyday life in the asylum, and she was not only there when
there were some very abusive practices but also when there was reform. There
was a physician named Dr. William Fletcher, and like all of the doctors she
mentions, this doctor had been in the Civil War. He was a great reformer. He
took all the restraints in the hospital and burned them in a giant bonfire on
Christmas Day of 1883. It made all the newspapers around the Midwest. She
described this. Dr. Fletcher brought in many reforms. He hired the first woman
doctor at the hospital. There were only twenty-two women doctors in state
mental hospitals around the country in the 1880s.
It turns out that six very clearly had bipolar
disorder and the other two might have. I was somewhat surprised by that, and
then went back and looked at other literature. There does seem to be an
association between bipolar disorder and creativity. A lot of well-known
musicians, writers, poets, and artists suffer from bipolar disorder. However,
the books we looked at were by ordinary people. I think one reason is because
their illness remits, so they write when they are well. The thing that I
enjoyed about the book that was written by the patient that write about was that
it wasn't just a polemic. Usually, people are complaining about abuses-with
excellent reason. She tells the awful stuff and the good stuff. She gives us
an insight into the everyday life in the asylum, and she was not only there when
there were some very abusive practices but also when there was reform. There
was a physician named Dr. William Fletcher, and like all of the doctors she
mentions, this doctor had been in the Civil War. He was a great reformer. He
took all the restraints in the hospital and burned them in a giant bonfire on
Christmas Day of 1883. It made all the newspapers around the Midwest. She
described this. Dr. Fletcher brought in many reforms. He hired the first woman
doctor at the hospital. There were only twenty-two women doctors in state
mental hospitals around the country in the 1880s.  Al: What do you think the patient/author's motivation to write her detailed journal
of her life at the time in the asylum?
Al: What do you think the patient/author's motivation to write her detailed journal
of her life at the time in the asylum?
 Al: Give me an idea without giving me the end of the story what her day would be
like?
Al: Give me an idea without giving me the end of the story what her day would be
like? Al: Is the building or institution still in existence?
Al: Is the building or institution still in existence?
 Al:
What is the societal responsibility for people who do not want to be
institutionalized. We refer to them as street people who are at risk but are
reluctant to accept treatment or assistance.
Al:
What is the societal responsibility for people who do not want to be
institutionalized. We refer to them as street people who are at risk but are
reluctant to accept treatment or assistance.  Al: Is there a specific country that would be a typical model for America?
Al: Is there a specific country that would be a typical model for America?
 I had the experience last fall of falling and breaking
my kneecap. I had to be in the hospital four days and have surgery. Now, as a
physician, I am very accustomed to hospitals and know how to deal with the
system. I was at a university hospital, had excellent care; a coordinator came
into set-up outpatient stuff, but she didn't get there the last day. The
physical therapist came, but not until the last day. So, when I got home, I
started calling around over a few days and finally found out that I was in their
computer; the people at the hospital got in touch with somebody else, who got me
in touch with somebody else. I finally got a nurse to come in and check the
dressing, got a physical therapist, but they didn't do basic home healthcare. I
have steps in my home, and the orthopedic surgeon was upset about my using them
with a leg immobilizer and crutches. I just wanted someone to come in to help
me with that, and we got another group to get a home health aide who came in and
helped me with chores. How many sixty-nine-year old women in this country have
this kind of care? I had "Cadillac" care, but the majority of people in this
country do not. Even with the best possible care, it is fragmented. It was
only because I'm a fussy old maid and got in there and screamed and yelled that
I got it organized for myself. However, this is not available to people who may
be working very hard, but have terrible health care benefits. I know the
system; I've worked it for forty years. I thought, my gosh, this is wonderful
for me, but what about all the others?
I had the experience last fall of falling and breaking
my kneecap. I had to be in the hospital four days and have surgery. Now, as a
physician, I am very accustomed to hospitals and know how to deal with the
system. I was at a university hospital, had excellent care; a coordinator came
into set-up outpatient stuff, but she didn't get there the last day. The
physical therapist came, but not until the last day. So, when I got home, I
started calling around over a few days and finally found out that I was in their
computer; the people at the hospital got in touch with somebody else, who got me
in touch with somebody else. I finally got a nurse to come in and check the
dressing, got a physical therapist, but they didn't do basic home healthcare. I
have steps in my home, and the orthopedic surgeon was upset about my using them
with a leg immobilizer and crutches. I just wanted someone to come in to help
me with that, and we got another group to get a home health aide who came in and
helped me with chores. How many sixty-nine-year old women in this country have
this kind of care? I had "Cadillac" care, but the majority of people in this
country do not. Even with the best possible care, it is fragmented. It was
only because I'm a fussy old maid and got in there and screamed and yelled that
I got it organized for myself. However, this is not available to people who may
be working very hard, but have terrible health care benefits. I know the
system; I've worked it for forty years. I thought, my gosh, this is wonderful
for me, but what about all the others? Al: And the thing is that we will see that healthcare cost in our insurance premiums to us directly.
Al: And the thing is that we will see that healthcare cost in our insurance premiums to us directly.
 Al:
It was interesting, the group got into a little bit of a heated discussion about
whether or not alcoholism was a choice.
Al:
It was interesting, the group got into a little bit of a heated discussion about
whether or not alcoholism was a choice.